Transgender Health
Callen-Lorde provides an affirming environment where patients can receive hormone therapy as well as engage in an ongoing relationship with a primary care provider and/or a mental health provider to address the full spectrum of health and wellness needs.
Callen-Lorde also provides Care Coordination tailored for patients that need additional support. Our Care Coordinators offer information, assistance and referrals regarding benefits and entitlements, including insurance, housing, and referrals to other supportive services.
Trans Health Services include:
- Primary Care
- Chest/Breast Health
- Hormone Care
- Pelvic Wellness Exams; PAP Tests
- Sexually Transmitted Infection (STI) Screenings & Treatment
- HIV/AIDS Testing, Treatment & Prevention, including PrEP and PEP
- Harm Reduction Counseling
- Care Coordination
Trans Health Resources
TransAtlasTransAtlas is a map-based guide to community organizations, agencies and spaces across the 5 boroughs of New York City, made by and for people of transgender, non-binary and/or intersex experience.
Drawn from Callen-Lorde’s Transgender Resource guide and Surgeon guide, and made by a team of transgender folks, TransAtlas maps hundreds of services and organizations across the 5 boroughs where TGNB folks can find trans-competent and friendly resources to help with anything from primary care to hair removal, addiction support, and religious institutions. You can search through dozens of surgeons, therapists, dentists, lawyers, barbers, case managers and more. Or try using our map to find social services near your work or home at your convenience.
How do I access gender affirming surgery as a Callen-Lorde patient?
Callen-Lorde does not provide gender affirming surgery for patients, but we can help you navigate the process, including:
- Finding a surgeon
- Insurance navigation
- Information about surgical procedures
- Care planning for your upcoming surgery
- Support letters from your PCP and mental health providers for insurance coverage
The first step to navigating the surgery process as a Callen-Lorde patient is to talk to a Callen-Lorde Medical Provider to complete a Gender Affirming Perioperative Services screener. You can schedule a virtual appointment to do this by calling our office at 212-271-7200 and confirming the surgery you are coordinating, the surgeon you’ll be seeing and the insurance coverage you’ll be using.
Finding a surgeon
It’s important to find a surgeon that you feel safe with, is accessible to you, and has experience in the surgery that you’re looking for (Safety, accessibility, experience). We encourage folks to consider scheduling consultations with a couple of different surgeons to be sure your needs are addressed. Check out the Callen-Lorde TransAtlas for a list of community resources and surgeons that perform gender-affirming procedures! https://transatlas.callen-lorde.org/
Insurance navigation
When we know the insurance plan we will have at the time of surgery, we can plan for the documents and requirements that we will have to provide insurance for the procedure, testing and appointments around surgery to be paid for. There are several different plans that we may qualify for depending on employment and income. Callen-Lorde’s Facilitated Enrollment team can support patients in signing up for insurance.
Information about surgical procedures
Patient education sessions with a GAPS Surgery Doula discuss specific procedures, preparation for surgery and recovery, and community resource referrals. Patients may also be scheduled for these appointments to discuss insurance needs and questions about selecting a surgeon or preparing for a consultation. You can schedule a patient education appointment with a GAPS Surgery Doula by calling our office at 212-271-7200 and letting us know what you would like to discuss with a surgery doula.
Learn about Callen-Lorde’s surgery navigation processes here
Binding and tucking are just two ways that TGNB people may choose to use to aid in their gender expression. Learn the do’s and dont’s in our helpful brochure series.
Methods
Layering Shirts
Wear a tight-fitting shirt as a base layer. Each shirt should get looser as you layer. Buttonup shirts work well as a final step to hide your chest. Layering shirts can be less restrictive, however, more clothing can become hot. Try moisture-wicking fabric for sweating.
Sports Bra
You can wear a sports bra under one shirt, or layer shirts on top of sports bras. There are many types of sports bras. Ones with higher Lycra content compress better. Try them on at a sporting goods store if possible. Average price: $25–$50.
Athletic Compression Shirt
Athletes wear these to aid in muscle recovery. They’re usually made from Spandex or Lycra, and are designed to absorb sweat away from your body. They typically work better for folks with less chest tissue. Companies like Underarmour and Sweat It Out sell them. Those with larger chests might want to try a medical compression shirt or binder. Average price: $20–$50.
Binder / Medical Compression Shirt
Binders offer even more compression than the above methods. Many are designed for people recovering from breast tissue surgery, but today there are companies who design specifically for transmasculine/non-binary folks. Some companies who sell them are Underworks, The Tool Shed, Moms Designs, Nouvelle, T.Kingdom of Taiwan, The Double T, Esha, and Danae. Prices range from $30– $100+ but if you can’t afford that, consider applying to a used binder program (listed in this pamphlet) for reduced prices or free!
Fitting
Chest Size
Measure the fullest area of your chest.
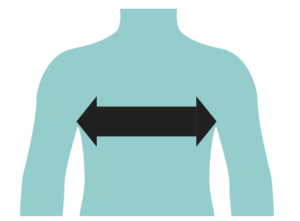
Binder Size
Look up the “sizing chart” of the company you’re buying from. If you fall between sizes, most people are more comfortable going a size up.
*Example sizing chart from underworks, sizing charts may vary depending on the company.
Low Cost Binders
The following programs offer binders for free or reduced cost:
GC2B Binder Program uppercasechase.com/binders.html
Point Of Pride Pointofpride.org/chest-binder
In a Bind inabind.transactiveonline.org (up to age 21)
Big Brothers Used Binder Program thetransitionalmale.com/BBUB.html
Binder Boys facebook.com/binderboys
Tumblr Transgender Clothing Exchange transclothesexchange.tumblr.com
Point 5cc T-shirt Company point5cc.com/chest-binder-donation
More Info/ Instructions & Tips Chest Binding 101 transguys.com/features/ chest.binding
Binder Reviews chestbinders.wordpress.com
Comfort Tips
Avoid Using Duct Tape And Ace Bandages
They can cut into skin, restrict breathing, and damage or even break ribs.
Kt (Kinesiology) Tape
This tape can be used to bind the chest but do not wrap it all the way around the body.
Give Your Body a Break
Binding while you sleep can further crush chest tissue and restrict breathing. Try to only wear it 8–12 hours at a time.
Make The Most of Your Break
Be sure to practice breathing exercises and stretch your arms and chest when not bond.
Smaller Isn’t Better
Binders are already designed to be tight. Getting one even smaller causes injury and discomfort.
Air It Out
Sweating under binders can lead to rashes, sores and chafing. Try wearing a thin undershirt or non-irritating body powder (like Gold Bond) underneath it.
Regularly Wash and Air-Dry Binders
This will help prevent irritation.
Lay it Flat
If your binder rolls up around the waist, try sewing a piece of fabric along the bottom that you can tuck into your pants.
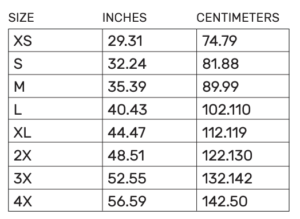
What is Tucking?
The goal of tucking is to make the underwear area look smoother. This can be done in multiple ways.
Why Do Some People Tuck?
- Tucking can help relieve gender dysphoria or make you feel better about your body
- Tucking can make wearing some shorts, skirts, and pants more comfortable
- Tucking can help you navigate situations more safely
So Where Does it All Go?
Some people prefer not to use anatomical terms to refer to their genitals, so from here on we’ll call the parts “PB & J.” There are spaces in your pelvis (called inguinal canals) right above your genitals that you can use to make your underwear area look flatter. You can push the PB up into these spaces and pull the J back. After you have been on hormones for a while, things will shrink and become more comfortable. This can all be secured using either medical tape or various clothing options.
Ways to Tuck
Control Brief s $10–30
Often marketed for “tummy control,” control briefs (like SPANX) are made of strong, elastic material. Pull yourself toward the back between your legs and pull the control briefs up snugly. You might have to readjust throughout the day. Some people prefer buying a size smaller than usual. Another option is cutting the legs off a pair of panty hose and wearing them like control briefs.
Layering Undies $10–30
Layering spandex undies might cause more irritation, so use cotton. Pull yourself toward the back between your legs and pull the underwear up snugly. Low waist/”hipster” styles don’t work as well.
Taping $5–10
Avoid using duct tape, see “Comfort Tips”. Wrap medical tape around the shaft and pull it down toward the back. Use more tape to secure. Medical tape removes less painfully, but does not stick when wet. Taping could make it painful to sit.
Gaff $20–30
Gaffs are worn like underwear and made of strong, elastic material to hold things in place.
Vee String $200–500
Vee Strings are like gaffs but are made of latex rubber and the outside looks like a vagina.
Comfort Tips
- Trimming/shaving generally helps with tucking.
- Use a sharp razor and shaving cream or soap to avoid irritation.
- Duct tape is not recommended because it can tear hair, skin and cause rashes or irritation. However, if you do use duct tape, remember to shave (although not right before, as that can cause irritation) so that the tape does not pull hair. Soak in a warm bath before removal to make the tape less sticky.
- It’s not possible to urinate while taped, so use the bathroom before you tape.
- Don’t forget to drink water, but try to make time to relieve yourself before and after.
- Remaining taped for longer than 4–8 hours causes irritation, discomfort, and possible pain while urinating. Try not to tuck 24/7. Take breaks if you can.
What Is Bottom Growth?
Bottom growth occurs when individuals who are transitioning experience clitoral growth after starting HRT therapy. While it’s common, it’s often not talked about.
What Happens During Bottom Growth?
Patients who go through bottom growth might experience increased sensation, vaginal atrophy and dryness, a higher sex drive and gender euphoria.
Maximizing Your Experience
For increased sexual pleasure, Callen-Lorde’s associate director of medical education Chance Krempasky, FNP recommends patients try “pumpking” (also known as “clit pumping”) or “vacuum-stretching.” Other experts suggest DHT cream as a more permanent way of increasing bottom growth or getting bottom surgery but this is not easily avialable in the United States.
If you don’t want to experience growth, Krempasky recommends that taking finasteride, which lowers DHT levels in the body, might help, but we don’t have the research to know for sure.
More Resources
For more information about this process, check out this Them article which features Krempasky’s expert voice.
Keep It Healthy
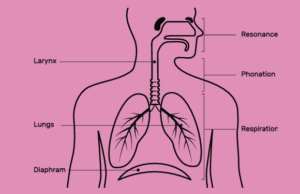
Where Does Voice Come From?
The health of your voice and vocal tract is important. This includes the health of your mouth, teeth, tongue, throat, larynx, and vocal folds.
A Healthy Voice is Maintained by:
- Reducing or eliminating smoking
- Reducing or eliminating alcohol or caffeine
- Drinking enough water to stay hydrated! Room temperature water is best.
- Treating acid reflux/heartburn if necessary
- Reducing excessive use of your voice on a daily basis (lecturing, singing, acting, etc.)
- Avoiding voice strain
- Resting your voice when necessary
Keep in Mind
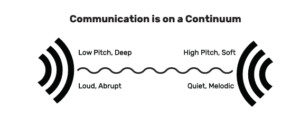
Don’t solely focus on changing the pitch of your voice— there are many other communication cues that can help affirm your gender!
Make It Yours: How Can The Way I Communicate Affirm My Gender?
Through Consistent Exercises That:
- Change social norms of speech
- Vocabulary, politeness, directness, emotional expression, etc.
- Change aspects of communication
- Articulation (like pronunciation)
- Pitch (how high or low the sound is)
- Duration (the length of your words, sentences, speech)
- Intonation (the melody of your speech)
- Resonance (how deep, loud a voice sounds)
- Voice quality
- Non-verbal cues (eye contact, facial expressions, gestures, posture, touching)
Getting Started
Diaphragm Breathing Exercise
Practice daily for just a few minutes! Sit tall as if a string is pulling up your body and relax your shoulders.
- Start by placing a hand on your chest and a hand on your stomach.
- Push out your stomach and fill your lungs with air. Imagine there is a candle in front of you.
- Pull your stomach in and breathe out for a count of 3 seconds as if blowing out the candle. Be sure your chest does not move as you breathe out
Laughing
Feminization
Higher pitch, more horizontal lips (less space, wide smile), quieter, say “ha” Masculinization: Lower pitch, more vertical lips, louder, say “heh”
Speech Feminization Exercise
to warm up your voice, adjust breath control, and vary pitch.
- Start by putting your lips together and blowing out air between them. (You want your lips to vibrate). Do this about 10 times.
- Next, slide your pitch up a little and then down a little as you continue to vibrate your lips.
Speech Masculinization Exercise
To increase resonance (increases the space in your mouth/ throat) and relax the muscles for speech.
- Open your mouth/throat wide as if you are about to yawn.
- Say “one, two” counting to ten.
- As you practice, speak louder and blend the sounds. You can yawn, sigh, or use an exaggerated “L” sound to open up your throat, such as in the word “Lollipop.”
For additional speech tutorials, look on YouTube!
Resources
NYU Speech-Language Hearing Clinic
665 Broadway, 9th Floor, New York, NY 10012
https://steinhardt.nyu.edu/csd/clinic
Ask about free group therapy or reduced price individual sessions. Teens must be accompanied by a guardian to receive services.
Voice Training:
EVA (Exceptional Voice App) exceptionalvoiceapp.com
Pitch Exercises and Ear Training: vocalist.org.uk
Tips for Voice: looking-glass.greenend.org.uk
Youtube Videos for Trans Women
Voice Training for Trans Women— Our Trans Journey
Male to Female: Voice Feminization
How to Talk Like a Girl Youtube
Videos for Trans Men
FTM: How to Lower Voice Pre-T
Transitioning as a Singer
Disclaimer
This information should be used as a general guide and should not be substituted for direct care from a qualified professional. This resource can provide information for individuals to work independently. If you have any healthcare issues that may interfere with the use of your voice, you should consult a healthcare provider before engaging in any exercises. Permanent and severe damage to your vocal anatomy can occur. Be aware of signs of vocal disorders: difficulty swallowing, uneven voice, vocal fatigue, loss of range, hoarseness or pain, and throat discomfort among other symptoms. If you experience these symptoms or any discomfort, you should see your doctor immediately; you must not participate in speech therapy with a professional or by yourself!
Keep In Mind
The target for changing communication is up to the individual. Starting point and goals may vary based on an individual’s vocal structures, cultural norms, and personal preference. There is no specific kind of communication you need to achieve! It is just important that you stay healthy and comfortable with whatever you choose.
Currently there are no comprehensive materials in the United States that focus on transmasculine people who have sex with men (TMSM). The term TMSM is being used here to include a wide range of identities including transgender men, non-binary assigned female at birth (AFAB), trans masculine individuals, and men with a transgender history. The pronoun “we” appears throughout this text because many of the authors identify as members of this community, and are impacted by these issues. We also recognize that some TMSM, and some who are not TMSM, have sex with trans women and transfeminine people, and that those of us who do have both overlapping and distinct needs from TMSM who have sex with men.
This booklet was produced with input from TMSM communities and experts in trans care who came together to provide this information with you in mind – from trans providers to our trans patients – for us, by us. Our goal is to discuss sexual health for TMSM, which is inclusive of all who fall under this umbrella, regardless of surgery or hormone status. The booklet will cover all aspects of sexual and reproductive health including fertility, pregnancy and contraception, safety in navigating men’s sexual spaces, sex work, disclosure, and sexually transmitted infection (STI) testing, treatment and prevention. We will also discuss gender affirming surgeries that could affect our sexual health, and general preventive care including cancer screenings and vaccinations. This resource is focused on the TMSM population because all MSM have higher risks of Human Immunodeficiency Virus (HIV) infection and STIs. Trans and nonbinary people may also not have the information necessary to make informed decisions about contraceptive options, especially if they are using testosterone. The booklet will include medical advice for TMSM about optimal health care so that they can advocate for themselves regarding their overall sexual wellness and pleasure.
Thank you for picking up this booklet. It is about the sexual health, sexual pleasure, and overall wellness of trans masculine people. We use this term as the best availible umbrella term for those who are female-assigned at birth and are living out their lives in a more expansive identity, which could be butch, nonbinary, two-spirit, being a trans man, or something else. We will use “trans” as a shorthand for these diverse identities. We hope this book is for you no matter what you’ve done to transition: if you’re taking hormones, or not on hormones, or have had surgery, or have not had surgery. No matter how you identify or what you’ve done to make your body a more comfortable place to live, our hope is to start a conversation with you about sex and your health.
We want to talk about the things that are important to you about being trans and having sex. We all may relate differently to what is in our pants, have different things there, and use them in completely different ways. We want to talk about this in a way that is simple and affirming – sometimes we may use medical language so we can be specific about what we’re saying, but we will try to use non-gendered words to talk about what is below the belt.
We also talk a lot about the risks and benefits of different choices about drugs, sex, and other topics where there is no one right way to behave, and each person makes their own individual choices. Our intention is to help you know how to take care of yourself better. Everything you do to help make yourself more comfortable in the world is important. We hope this booklet helps you be as safe as possible while navigating the world as a trans person.
Sexual Pleasure & Health Resource Guide for Transmen who have Sex with Men
Hysterectomy is commonly used to refer to removing all internal reproductive organs: the cervix, uterus, fallopian tubes and ovaries, although technically “hysterectomy” only means removal of the uterus.
Removal of the vagina (vaginectomy) is not a required part of hysterectomy or other genital surgeries (metoidioplasty and phalloplasty), but if you are planning to get a vaginectomy, hysterectomy will be performed in advance or at the same time.
If the cervix is removed, you no longer need to get monitoring pap smears.
Some people choose to leave one or both ovaries in the hope that they can function as internal estrogen hormone production when someone chooses to stop taking testosterone or loses access to testosterone.
Long term, you need to have either testosterone or estrogen in order to maintain bone density and for energy and mood.
Some people choose to leave ovaries in order to retain material to genetically reproduce with later.
Reduction vs Reconstruction
Reduction and reconstruction surgeries look to remove tissue and skin to create a flatter chest.
Reduction surgery removes little to some of the tissue from the chest. Some skin may be removed to sup- port and contour the tissue that remains.
Reconstruction surgery will re- move some to most of the tissue from the chest. Skin on the chest is removed and contoured along our pec muscles.
There are different types of reduction and reconstruction procedures that we can choose from based on the amount of tissue we need to remove.
Reduction
Reduction procedures are ideal when we expect some of the tissue on our chest to remain after surgery.
Scarring can look different depending on the amount of tissue and skin that is removed. Depending on our surgeon, we may have options between inverted T scars, scars just under the chest tissue (along our pecs) or around the areola.
Our areola may be reduced in size to match the proportions of our chest. Depending on the amount of tissue removed and location of incisions, our nipple sensation may change or be slow to return after surgery.
Reconstruction
Reconstruction procedures are ideal when we expect most of the tissue on our chest to be removed during surgery.
Scarring can look different depending on the technique we discuss with our surgeon. Depending on our surgeons’ experience we may have the option to choose between double incision, keyhole/ peri-areolar, fish mouth, and inverted T techniques.
Nipple grafts, or parts of our nipples and areolas, are removed then resized and placed back in a lower and outer facing direction. Before surgery the surgeon draws guides on our chest to be sure they line up as best as possible after recovery.
Also known as ‘Facial Feminizing Surgery (FFS)’ or ‘Facial Masculinizing Surgery.’ These are a collection of procedures designed to change the bone structure of the face and reshape features that resulted from our first puberty.
Surgical Facial Procedures could include bringing the hairline further forward, shaving down or entirely recontouring the forehead and sinus area by cutting and repositioning bones (osteotomies), shaving the jaw line or reducing and repositioning of the jaw bone (a reduction or sliding genioplasty), lifting the upper lip, nose reconstruction or a ”nose job” (rhinoplasty), fat grafting, implants and tracheal shave (cricothyroid cartilage reduction).
The same procedures can be performed in reverse for masculinization.
Non-Surgical Facial Procedures could include the use of injectable or topical treatments to address scarring from shaving or previous facial procedures, hair growth or restoration or as an option for folks that cannot access surgical procedures at this time.
Vocal surgery can raise the pitch of the voice, but it may also reduce vocal range.
Insurance and surgeons usually require Vocal Therapy before and after vocal surgery. Some of us may have significant results from vocal therapy alone and choose to not have surgery. Vocal surgeons usually have therapists that they refer patients to and are familiar with their requirements for preparing for surgery. These visits help us work with our vocal cords to change the vocal range of our voices when we speak. They also help prepare our bodies for recovery and the vocal therapy that is required to complete after surgery. Speech-Language Pathologists have special training to prevent vocal misuse and vocal damage.
Vocal surgery can raise the pitch of the voice, but it may also reduce vocal range. Total Vocal Rest for up to a few weeks is standard for recovery from these procedures. Complications can include having a raspy or strained voice after surgery.
Phalloplasty uses a piece of (non-genital) skin that is fully removed (free flap) or partially removed (pedicled flap) and then re-attached to the genital area to create a penis.
Depending on the surgeon, phalloplasty can be completed in a ‘single stage’ or multiple stages. Regardless, if we are seeking an erectile device and/or testicular implants, we will need at least two surgeries, if not more.
Going through all of the surgeries involved with phalloplasty can take at least 1-2 years, but for many people it can take longer than that. We should also factor in time for replacing erectile devices every few years as well.
Phalloplasty can be combined with:
- Urethral lengthening
- In order to stand to pee
- Usually performed by a surgeon who has completed a reconstructive urology fellowship
- Vaginectomy
- Removal of the vaginal opening
- Scrotoplasty
- Creation of a scrotum or ballsack
- Glansplasty
- Creation of a ridge or head of the penis
- Mons reduction
- Pubic area lift and debulking
- Insertion of testicular implants and erectile device
Metoidioplasty (‘Meta’): frees the existing erectile tissue by cutting the tissue that holds it down against the body.
The penis might be enhanced by using nearby tissues to create more girth in “ring” and “centurion” methods, but generally length is dependent on growth from testosterone.
The penis can also loose length post op.
- No additional donor site, no large area of scarring
- Low risk of loss of sensation
- Often able to achieve unassisted erection
- Fewer stages
- Generally only 1-2 surgeries
- May or may not be able to have penetrative sex depending on personal anatomy and growth from HRT (53% chance of being able to)
Metoidioplasty creates a small penis made out of the clitoris. It is usually done in one step, meaning one visit to the operating room (OR). The penis can become erect and stand up, but is usually between 1 and 2 inches in length. The penis size depends on the size of the clitoris before surgery, and how much it grows from T. Some of us use methods like pumping to try to get more growth.
Many people have injected free silicone in their body. Most people get silicone injected into their body to create curves in their hips and buttocks, create more feminine cheekbones or facial features, or to make their breasts bigger.
Silicone injections are approved in the US only for treatment of certain eye disorders. Some doctors inject silicone into other parts of the body. Others, who may not be licensed medical providers, may say they use “medical grade” silicone for injections, but there is no way to know what is actually being injected. Regardless of who is injecting or what is being injected – silicone injection in the body can have dangerous health effects.
What is silicone?
- Silicone can be a free oil or can be in a capsule, like a breast implant.
- If it was put in your body with surgery, it is an implant.
- If it was injected, it is free silicone. Injected or free silicone sometimes is mixed with harmful substances such as bathtub caulk, motor oil, cooking oil, mineral oil, or cement glue- even it was described as “medical grade.”
What do health professionals say about silicone injection?
Most medical professionals and the Federal Drug Administration (FDA) agree that silicone injection is dangerous.
What are the potential complications from silicone injections?
- Silicone can cause infection after it is injected, and might cause life-threatening blood clots, including a condition called pulmonary embolism where a blood clot gets stuck in the lungs.
- As silicone ages in the body, it can move to different areas (migration), like silicone in the hips falling down into the ankles or silicone in the cheekbones falling down into the cheeks.
- Silicon can also cause severe pain as it shifts and moves.
- Silicon hardens as it ages and may create hard knots (granulomas) under the skin and a dimpled appearance of the skin.
- Silicone can be very difficult to remove once it has been injected, which means that these changes may cause chronic pain and other health complications.
Is there anything I should be doing now if I have already injected silicon?
- Being aware of the possible complications related to silicone injections (such as those listed above) and recognizing these symptoms is an important first step in seeking appropriate treatment.
- Not knowing what’s going on with your body and the silicone inside it can be scary. Talking with a knowledgeable medical provider is important.
- Your provider can also check whether your silicone is causing side effects by doing certain blood tests including calcium and markers for inflammation. But there are other things, like HIV, that can cause these labs to change.
- If you got your silicone a long time ago, and it’s not bothering you, it’s probably ok to keep it.
- If you are in pain, you can ask your medical provider for treatment of your pain.
Should I get my silicone removed?
The short answer is maybe.
- You don’t have to remove injected silicone if you don’t want to!
- Silicone removal may require surgery. Surgeons often have physical requirements before they operate. For instance, if you have a chronic condition like diabetes or HIV, they will want to see information showing those are being well-controlled. Some surgeons have weight limits, and many will not operate on people who smoke cigarettes. They may check your urine (pee) for nicotine from any tobacco source.
- There is no such thing as the perfect patient for silicone removal. Surgeons will look at your body, where the silicone is placed, how deep or shallow it is, and your health overall.
- It may be more dangerous to get silicone removed than to leave it in your body for the long term.
- It is still possible to have pain after silicone is removed.
- It is also difficult to remove silicone and trying to take it out can cause skin problems, wounds that don’t heal, and disfigurement. After removal there is a dip inward where the silicone was making a curve before.
- Everyone has to make their own decision about silicone removal. You do not need to remove silicone unless it is causing very bad pain or other medical problems.
- If you are in pain, you can ask your medical provider to treat your pain. If you would like it removed, you can ask your medical provider for more information.
If I choose to get it removed, what does that process look like?
How to get rid of silicone is a process that depends on how much of it you have, where it is, and what is happening with it. There may be imaging (CT scans) required.
Where can I learn more?
- Ask your primary care provider about the options that might be available to you.
- If you are seeking or already have sought gender affirming surgery, ask your surgeon for more information about what services they might provide.
- You can also learn more about surgeons who might provide silicone removal at transatlas.callen-lorde.org
What does it cost?
- Insurance will only cover silicone removal if it is causing problems that keep you from living your life. If you are not having major problems from silicone, you may have to pay for surgery yourself.
Warnings from community members
Avoid injecting silicone into the legs and feet. For example, silicone injected under the feet to make wearing high heels more comfortable can result in the same long-term problems as silicone injected anywhere in thebody.
Cortisone shots do not provide lasting relief for the discomfort caused by silicone injections, and could be harmful.
References
FDA Warns Against Use of Injectable Silicone for Body Contouring and Enhancement: FDA Safety Communication
Sergi, Francesco D., and Erin C. Wilson. 2021. “Filler Use Among Trans Women: Correlates of Feminizing Subcutaneous Injections and Their Health Consequences. Transgender Health. 6(2): 82-90.See Sergi and Wilson. 2021
Download a PDF of this content here.
Here is the Spanish translation.
Pronouns Matter!
Callen-Lorde offers many resources to our TGNB clients and staff including pronoun stickers accessible at every front desk. Check out our video highlighting the Pronouns Matter campaign and see how the use of a person’s correct pronoun can lead to a more welcoming, safe and respectful atmosphere for everyone.